Health, wellbeing and clinical care
Imposing quarantine on people can mean they are caught without their usual health resources and support.
Early in the COVID-19 pandemic, health systems were strained leaving many repatriated residents without access to routine care prior to their arrival in Australia. In addition, the unknown aspects of the virus and the isolation of quarantine exacerbated and/or instigated mental health problems.
In alignment with a resident-centred quarantine model, the facility has a duty of care to ensure the resident has:
- 24-hour access to emergency treatment.
- Medication and treatments vital for their ongoing health and wellbeing.
- An environment conducive to mental health and wellness.
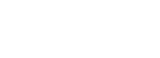
The Centre for National Resilience, Howard Springs Quarantine Facility differed in presenting a health-led model of quarantine, described as a quarantine facility with a primary health care overlay.
Quarantine facility with a primary health care overly
This section presents an overview of the quarantine facility actions and strategies to promote health and wellbeing on-site for both staff and residents.
The quarantine service is recognised as a separate entity to secondary (speciality services) and tertiary (acute services) clinical facilities however, it is not registered as a primary health clinic and therefore not subjected to the same accreditation requirements as a clinical facility.
The quarantine service presented in this resource operates with a foundational primary health and wellbeing approach. It is situated with the Department of Health and is predominantly staffed by registered health professionals. The quarantine facility with a primary health care overlay considers the health and wellbeing of residents and staff as a core component of service delivery.
The quarantine facility is not able to support residents requiring a high level of care, and these residents are safer in a secondary or tertiary health environment.
Indicators for relocating a resident to a supportive health service include:
- acute level of infectious disease signs and symptoms
- shortness of breath
- chest pain
- signs of mental health instability which may result in danger to themselves or others
- unwell with multiple co-morbidities
- dependent on others for the provision of all care.
The facility needs to provide the environment, rooms and equipment for residents who may require additional support, such as residents living with a disability where the individual is well and self-caring.
Staff need to feel safe at work and have access to support services which are built into the quarantine service delivery structure. It is recommended all staff are required to have first aid and basic life support training prior to commencing their role. This adds a layer of safety to everyone on the site.
A core responsibility for the Health Leadership Team is to construct the policies, processes and strategies focusing on staff and resident health care.
The Health Leadership Team are expected to be active champions of the site’s Infection Prevention and Control (IPC) and Safety and Quality Committees. They are integral to informing the priorities for health and wellness and must be connected with the emergency operations centre and other core sectors and organisations which will lead the pandemic response.
Access the full resource for Section 5_Health, wellbeing & clinical care
Individual sections for health wellbeing and clinical care are presented with the information below.
A quarantine facility will present a full range of medical conditions ordinarily encountered in adults, women and children’s general practice. The Medical team focuses on managing health issues on-site as much as possible to avoid unnecessary transfer into the acute care system. This recognises that all residents onsite are considered potentially infected (unless a known positive case) and thus puts the health system at risk.
The Medical Team needs to be connected to the community and establish referral systems for residents to external health support (such as local general practitioner clinics). They are required to be proactive and reactive, contribute to the Quality Assurance and IPC Committees and remain current with disease trends.
The purpose of the quarantine medical team is to:
- Provide medical assessment, treatment, triage and referral for unforeseen and emergency medical needs among people undertaking supervised quarantine or isolation.
- Facilitate access to medication for residents in quarantine or isolation where this is unavailable from another source, such as a resident’s usual GP or telehealth consultation with a GP.
- Determine eligibility for viral (COVID-19) specific therapy and facilitate access to this treatment in accordance with Government Health guidelines.
- Quality assure the quarantine and isolation exits process for quarantine residents.
- Coordinate the handover and follow-up treatment of people exiting quarantine and isolation who have complex medical needs with welfare and medical teams outside of the quarantine service.
During the operation of the Centre for National Resilience, research was conducted on the healthcare needs of residents identifying the main health needs and priorities. This has been published and can be accessed here.1
A full outline of the responsibilities of the Medical Officer can be found in the following attachment. This includes a presentation of their core roles and responsibilities and the medical referral system.
- Auditing of IPC and PPE practices.
- Delivery of education and training across the site.
- Representation across health leadership teams, IPC and quality and safety committees and telewellbeing teams.
- Daily reporting of resident status with a priority on any residents of concern. This can be defined in many ways with the main specifics identified as:
-
- Residents who have known factors meaning they are more susceptible to disease
- Residents who have known medical or mental health conditions that may warrant further support
- Residents who have had medical referrals and may be under medical management.
-
The specialist team provides an important service for the quarantine facility.
This team consists of a Nurse Manager and Social Worker as team leaders with a full team structured in accordance with resident numbers and their anticipated needs. This includs physiotherapists, occupational therapists, additional social workers, drug and alcohol nurses, mental health nurses, a trauma nurse practitioner and welfare support. Additional Specialist Team members are strategically located with the Tele wellbeing services and consist of a mental health nurse and welfare services.
The Specialist team is included in the assessment of the resident in the pre-arrival process to review information that may initiate their team’s response. For example, residents who have provided notification about a disability or mental health concern. They are required to have representation at all resident arrivals to assist with the initial health screening of residents. This ensures aspects of concern such as mobility problems or evidence of anxiety are noted and addressed immediately or followed up as required.
The Specialist Team have a standard operating procedure and their own referral pathway to connect residents with their staff and services.
Further information about their team structure and service provision has been provided in the following document.
Government policy and legislation require health services (which extends to quarantine services) to ensure that people who cannot speak English, or who speak limited English, have access to professional interpreting services when significant decisions are required and when essential information is being communicated. Interpreters in Australia are accredited by the National Accreditation Authority For Translators and Interpreters.2 In certain circumstances, family members, or bilingual staff may also be used as interpreters onsite.
The site requires access to interpreters on a regular basis and where possible should prepare this access in advance aligned with the language and culture of the anticipated residents.
This information can be obtained for organised repatriation flights as part of the pre-arrival resident information. Effective care and support of residents depend on good communication. Inadequate communication with people who have limited English proficiency restricts their access to and understanding of quarantine and can have a profound impact on the quality of support and care they access.
Access the resource for Section 5 Interpreter services here.
2.National Accreditation Authority for Translators and Interpreters. (n.d.). NAATI Endorsed Qualifications. https://www.naati.com.au/services/endorsed-qualification/
- the face to face visits by the health staff was important for resident’s health and wellbeing,
- the open air balcony was a positive aspect of quarantine for residents,
- residents who became COVID-19 positive were managed well,
- staff observed other staff to be compassionate and caring of residents wellbeing,
- the residents were well cared for, and
- the rooms were comfortable for residents.
- Collaborate on resident care needs
- Store clinical and medical equipment
- Receive deliveries of medical equipment and medications
- Accommodate the Medication room
- Provide a treatment room
- Position the vaccine clinic
- Situate the pathology fridges for the collection of specimens (viral (COVID-19) swabs).
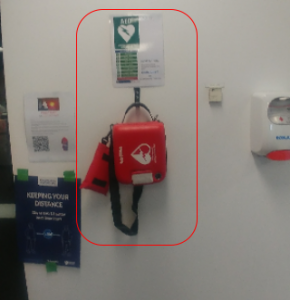 Health Team leaders are required to educate their staff on the location of AEDs and work through the process of accessing, checking and using these in the quarantine setting.
Having current basic life support which incorporates the use of an AED is considered mandatory for all staff. This ensures if an AED is required, staff are confident and competent to retrieve and use the AED.
Implementing an AED requires additional consideration of disease transmission risk and PPE as presented in the following section on medical emergencies.
Health Team leaders are required to educate their staff on the location of AEDs and work through the process of accessing, checking and using these in the quarantine setting.
Having current basic life support which incorporates the use of an AED is considered mandatory for all staff. This ensures if an AED is required, staff are confident and competent to retrieve and use the AED.
Implementing an AED requires additional consideration of disease transmission risk and PPE as presented in the following section on medical emergencies.Section 5: Figure 3: Emergency Codes used in quarantine.
| Code Red | Fire/Smoke | |
| Code Orange | Evacuation | |
| Code Blue | Medical Emergency | |
| Code Yellow | Facilities and Equipment Shut Downs and Overloads | |
| Code Purple | Bomb Threat | |
| Code Black | Aggressive Incident | |
| Code Brown | External Emergency | |
| Additional code added specifically for the quarantine facility | ||
| Code Green | Resident Absconded | |
References
- Harris.H., V. L. S. K. (2022). Mandatory, supervised quarantine of international travellers: Experience from the Centre for National Resilience [Observational Study]. The Quarterly(Q1), 24,25,26,27.
- National Accreditation Authority for Translators and Interpreters. (n.d.). NAATI Endorsed Qualifications. https://www.naati.com.au/services/endorsed-qualification/
- Sidebottom, D. B., Potter, R., Newitt, L. K., Hodgetts, G. A., & Deakin, C. D. (2018). Saving lives with public access defibrillation: a deadly game of hide and seek. Resuscitation, 128, 93-96. DOI: 10.1016/j.resuscitation.2018.04.006
Content acknowledgement
Content in this resource has been created and, in some cases, directly copied with permission from documents and resources owned and prepared by the Northern Territory Government, Department of Health, Centre for National Resilience, Howard Springs Quarantine Facility and the National Critical Care and Trauma Response Centre.
Reference this webpage (APA style guide)
To reference the webpage:
Charles Darwin University. (2023). Pandemic Quarantine Facility Guide. Top End Academic Health Partners. https://quarantine-guide.cdu.edu.au/
To reference a webpage document:
Charles Darwin University. (2023). Section 5 Health wellbeing and clinical care: Mental health and wellbeing. Top End Academic Health Partners. https://quarantine-guide.cdu.edu.au/wp-content/uploads/2023/04/SECTION-5-Mental-health-and-wellbeing.pdf
Pandemic quarantine facility guide abbreviations and full reference list.