Processes, infrastructure and communication
The Centre for National Resilience (CNR) provided a foundation to build recommendations for how a large-scale quarantine and isolation facility should approach resident quarantine and isolation care.
Through examination of the development and implementation of CNRs quarantine and isolation processes, infrastructure and communication models this Toolbox presents a number of evidence-based guidelines for adaption to any quarantine and isolation facility.
Each section incorporates the underpinning primary health care approach CNR adapted and is focused on 5 core areas providing guides for site, staff and resident management.
The Centre for National Resilience differed from other quarantine and isolation approaches in it was led by the Department of Health with a primary health foundation in service provision. The service was supported by the Department of Home Affairs, the Australian Defence Force, and private organisations (contractors) for day-to-day operations.
Core points of CNR processes and resident care are identified as:
- The site functioned with a resident-centred model of care incorporating a primary health approach, which promotes resident self-care with onsite referral and access to primary health services and established pathways for acute care services.
- Incorporation of core public health approaches for community safety and health promotion.
- Communicable disease transmission risk reduction and infection prevention and control integrated health strategies with aim to maintain overall health and wellness of residents and staff.
As the facility operates with a primary health foundation, the site may not need to be accredited as a registered health facility and therefore does not require the same accreditation and linkage with Medicare for the services it provides. The levels of health service provision incorporate primary health support to residents without functioning as a full primary health clinic with comprehensive primary health care management pathways (refer to Section 5 Health wellbeing and clinical care for a full overview of the health support provided to residents and staff onsite).
This section presents an overview of the core activities and communication considerations which form the basis of a quarantine service. These are expanded throughout the sections on infection prevention and control, health workforce, resident care and health, well-being and clinical care. Additionally, approaches and recommendations for the infrastructure and environmental aspects of a quarantine facility are provided.
Access the resource Section 1 Processes infrastructure and communication
On March 11, 2020, the World Health Organisation (WHO) declared the novel coronavirus (COVID-19) outbreak a global pandemic. In response, Australia’s borders were closed to all non-residents on 20 March 2020 and returning residents were required to spend two weeks in supervised facility-based quarantine from 27 March 2020.
The Northern Territory (NT) Chief Minister announced border restrictions for all access points into the NT from 24 March, 2020, with limited exemptions. In July 2020, the NT introduced mandatory, supervised quarantine for returned international travellers and for domestic travellers from declared Australian COVID-19 ‘hot spots’ who were eligible to enter the NT.
Two NT quarantine facilities (NTQF) were established – the Centre for National Resilience (CNR) in Howard Springs, Darwin, which provided quarantine of international, repatriation, humanitarian and domestic travellers; and the Alice Springs Quarantine Facility, Alice Springs for quarantine of domestic travellers. CNR operated under joint Australian and NT government governance from July 2020 until 15 May 2021, when facilities transitioned solely to the NT government’s management and oversight.
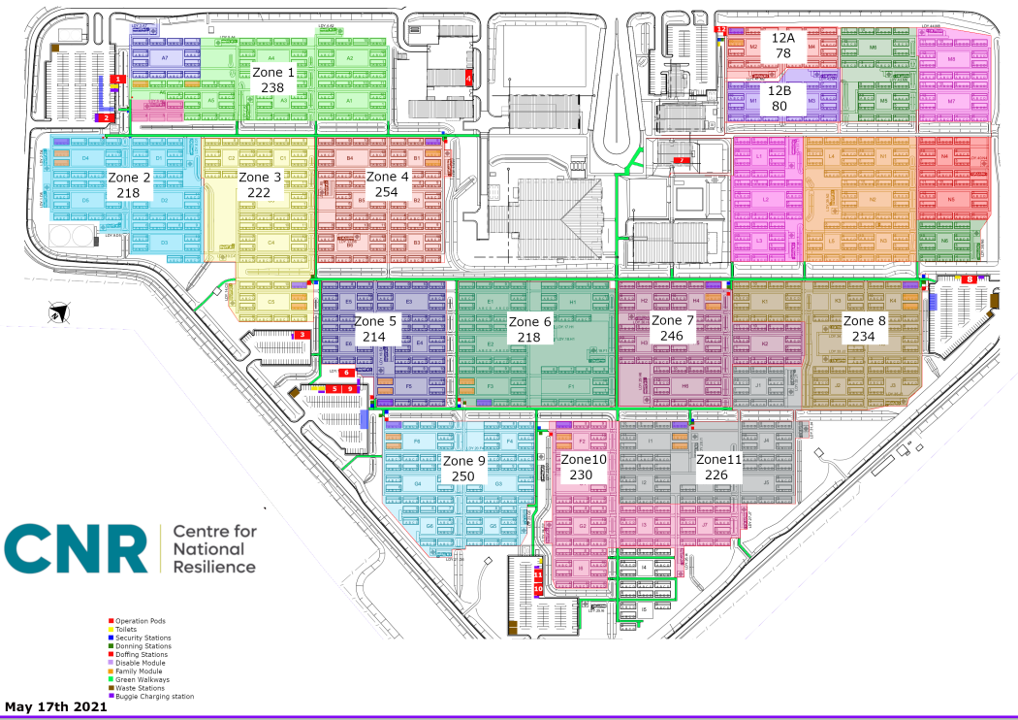
The Larrakia traditional owners of Darwin named the Howard Springs village Manigurrma, after the Larrakia name for the Stringybark tree used to build shelter in times past. The site is a re-purposed facility formerly used for mining accommodation. CNR can accommodate up to 2,700 returned travellers, and houses people in stand-alone portable dwellings, each of which has its own separate air conditioning and an outdoor verandah. CNR was divided into quarantine ‘zones’ so that cohorts of international travellers can be kept separate from one another, preventing mixing of people from different cohorts.
The Northern Territory Government (NTG) completed considerable work to expand the capacity at the Centre to support up to 2,000 returning Australians per fortnight. This included four critical dependencies for expansion: workforce recruitment and training, capital works at the Centre, transition to a single source of Centre management and streamlining the arrivals process (which included a transition to flight arrivals at Darwin International Airport). CNR developed into a core strategic pandemic response resource for Australia successfully quarantining 14,867 repatriated residents and 18,210 domestic residents with zero COVID-19 transmission recorded from residents to staff for the duration of its operation.
The Northern Territory Government (NTG) completed considerable work to expand the capacity at the Centre to support up to 2,000 returning Australians per fortnight. This included four critical dependencies for expansion: workforce recruitment and training, capital works at the Centre, transition to a single source of Centre management and streamlining the arrivals process (which included a transition to flight arrivals at Darwin International Airport). CNR developed into a core strategic pandemic response resource for Australia successfully quarantining 14,867 repatriated residents and 18,210 domestic residents with zero COVID-19 transmission recorded from residents to staff for the duration of its operation.

The purpose of mandatory, supervised quarantine
The overarching purpose of mandatory, supervised quarantine is to prevent communicable disease outbreaks in the community, reducing morbidity and mortality. To achieve this purpose, CNR prevented infection and spread of disease through comprehensive, evidence-based infection prevention and control practices which were rigorously adhered to by every person involved in the care and support of CNR residents.
This included:
- Systems and processes to ensure safe resident and staff flow and movement in and around the sites;
- Isolation and physical separation of infected cases and close contacts from other residents;
- Infection prevention and control through physical distancing, hand hygiene and appropriate use of personal protective equipment (standard precautions);
- Cleaning, disinfection and waste management;
- Comprehensive laboratory testing for communicable diseases for all staff and residents; and
- Emergency responses that minimise the risk of communicable disease transmission.
The service facilitated a way for Australians to return home as soon as possible with benefits extending to rebuild the country’s economy through increased economic opportunities; and by protecting Australians from any transmission of COVID-19 from returning Australians.
The following resource provides an overview of engaging with First Nations People with quarantine services.
Having coherent site processes which are clearly articulated for staff ensures the quarantine and isolation facility can operate safely and efficiently.
This section presents an overview of the core processes underpinning the quarantine service provision based on the operations of the Centre for National Resilience. Each subsequent section of the toolbox continues to present a comprehensive overview of site processes across: infection prevention and control, the health workforce, resident care, and health wellbeing and clinical care. Process start-up guides have additionally been presented in Section 1 to allow a quick overview of core quarantine and isolation facility operations.
This section introduces the main concepts in commencing a quarantien service with referral to the more comprehensive process overviews throughout the toolbox.
The quarantine facility’s infrastructure and general environment directly impact the functionality of the teams and the experience of the residents. During the COVID-19 pandemic, the lack of facilities appropriate for quarantine and isolation purposes was apparent and through a trial of using established structures, it became evident certain infrastructure characteristics were more conducive to infection prevention and control (IPC) measures and the health and well-being of staff teams and
residents. This highlighted building status in relation to ventilation, space capacity, and structures that promoted mental and physical health and wellbeing. For the Centre for National Resilience (CNR) an additional focus point was environmental factors associated with weather and climate with staff working outdoors in a hot tropical area.
This section focussed on the quarantine services site infrastructure is based on the infrastructure characteristics of the CNR which contributed to the success of the site as a quarantine facility. This includes environmental concerns and recommendations on quarantine service design from the wider pandemic.
The Work Health and Safety Team are situated with the Operations Team and are onsite to ensure there are safe work practices and infrastructure playing a lead role in the ongoing development of a culture of safety and reduction of work-related injuries (or in the case of quarantine transmission of infection). They are predominantly auditing the site to ensure they have safety standards that are aligned to those presented Work Health and Safety (National Uniform Legislation) Act 2011 and Work Health and Safety (National Uniform Legislation).1,2 The CNR was guided by the NTWorkSafe Codes of Practice supporting the strategic plan with the quarantine service falling into the health and community services industry area.
This section continues with the presentation of the site emergency management plan, WHS committee, risk management and general practices of the WHS team within the quarantine facility. An example of the WHS Team audit process for buildings and structures has been presented in Section 1 Site infrastructure & environmental considerations.
A coherent approach to communication across the quarantine service is required to ensure safe site practices. In the early stages of the COVID-19 pandemic, communication was challenging for Leadership Teams with decisions often being made in a reactive rather than proactive cycle to quickly establish systems and processes. This often requires innovative use of technology and resources to develop inclusive communication strategies with access to information, clear hierarchical structures, and feedback cycles.
This section presents an overview of the communication strategies for implementation in the quarantine and isolation facilities, inclusive of communication with residents, staff and communication tools.
This section of the toolbox provides start-up guides for the quarantine and isolation service processes. These are brief overviews that provide practical directions with links to the relevant toolbox section for further information.
| Quarantine and isolation processes | Description |
| Resident arrivals | Process for managing bus arrival of residents to the quarantine facility, safely checking residents into the facility and taking them to their rooms. Modelled on 50 or more residents arriving. Access the resource for Section 1 Process Start-up guide Resident Arrival. |
| Resident departure | Process for residents to safely exit the quarantine facility. Modelled on 50 or more residents exiting. Access the resource Section 1 Processes Start-up guide_Resident departure |
Personal protective equipment (PPE) training -Donning and doffing | Process to train staff in donning and doffing personal protective equipment (PPE) for contact and non-contact roles when entering resident red or orange zones inclusive of MEG (mask, eye protection and gloves) and GMEG (gown, mask, eye protection and gloves). Access the resource Section 1 Processes Start-up guide_PPE Training |
Viral screening process -Staff | Process for viral screening of quarantine facility staff. Access the resource Section 1 Processes Start-up guide_Staff viral screening |
Offical visitors to the quarantine service | Process for managing official visitors to the quarantine site. Section 1 Processes Start-up guide_Official visits to the quarantine service |
| General quarantine site cleaning | Process for cleaning general use areas across the quarantine site (not for red or orange resident zones). Access the resource Section 1 Processes Start-up guide_General cleaning |
References
- Northern Territory Government. (2020, Feb). WORK HEALTH AND SAFETY (NATIONAL UNIFORM LEGISLATION) ACT 2011. https://legislation.nt.gov.au/Legislation/WORK-HEALTH-AND-SAFETY-NATIONAL-UNIFORM-LEGISLATION-ACT-2011
- Northern Territory Government. (2022, May). WORK HEALTH AND SAFETY (NATIONAL UNIFORM LEGISLATION) REGULATIONS 2011. https://legislation.nt.gov.au/Legislation/WORK-HEALTH-AND-SAFETY-NATIONAL-UNIFORM-LEGISLATION-REGULATIONS-2011
Content acknowledgement
Content in this resource has been created and, in some cases, directly copied with permission from documents and resources owned and prepared by the Northern Territory Government, Department of Health, Centre for National Resilience, Howard Springs Quarantine Facility and the National Critical Care and Trauma Response Centre.
Reference this webpage (APA style guide)
To reference the webpage:
Charles Darwin University. (2023). Pandemic Quarantine Facility Guide. Top End Academic Health Partners. https://quarantine-guide.cdu.edu.au/
To reference a webpage document:
Charles Darwin University. (2023). Section 1 Processes, infrastructure and communication: Work Health and Safety. Top End Academic Health Partners. https://quarantine-guide.cdu.edu.au/wp-content/uploads/2023/04/Section-1-Work-Health-and-Safety.pdf
Pandemic quarantine facility guide abbreviations and full reference list.