Resident care
The effective and safe care of the resident is paramount in quarantine service delivery.
It is known that individuals can suffer from poor mental and physical health outcomes from isolation and in times of global pandemics there is associated fear and anxiety.
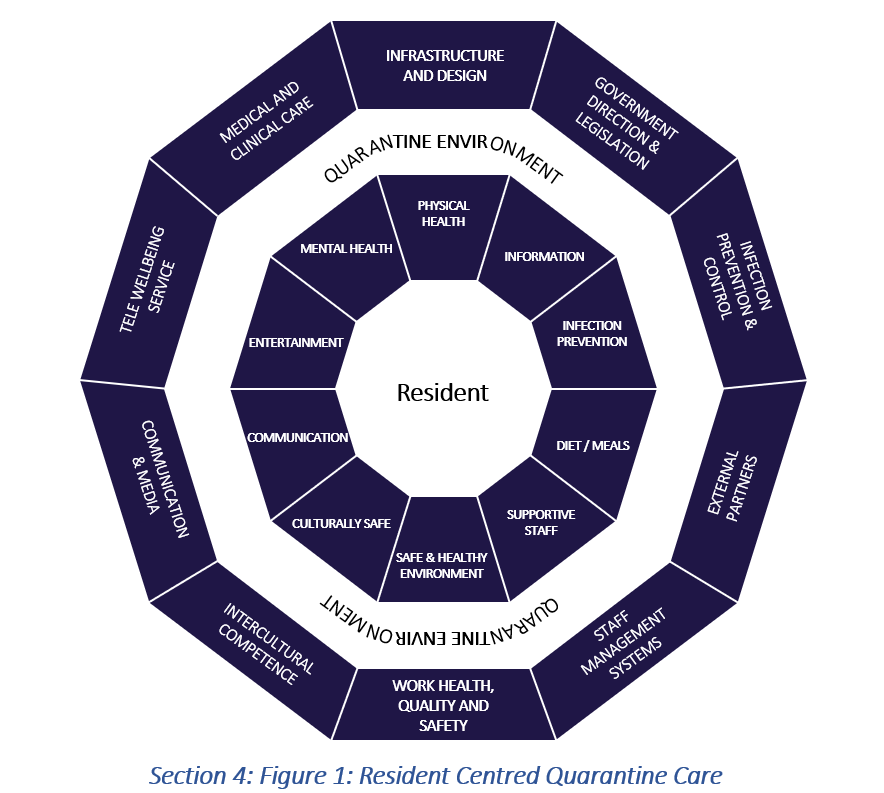
The recommendations for a resident-centred model of quarantine care ensures the health and well-being of the residents are prioritised and public health, infection prevention and control and other aspects of disease management are developed around the resident’s needs.
Resident-centred quarantine care
Access the full resource Pandemic Quarantine Facility Guide Section 4.
Individual sections for resident care are presented with the information below.
Resident centred quarantine care model
The resident care model is presented as 10 core areas (aligned with quarantine service provision) with links to relevant resources.
The physical health of people is intrinsically linked to overall mental health and wellbeing and is known to aid recovery from disease and prevent ill health.¹
Quarantine services have a duty of care to residents to provide for their primary health care needs.
It is reasonable to expect a level of self-care from residents for their health and wellbeing but quarantine services must also ensure they have easy access to primary care health support if required.
The primary health services normally accessed in the community, such as a general practitioner, filling medication scripts, accessing mobility aids or specific medical diets (such as a diabetic diet) need to be provided as part of the quarantine service model of care.
Complex medical care not within the scope of the quarantine facility needs to be assessed by the Health Team and where possible deferred until the quarantine is complete or arrangements are made for the care to occur in a suitable acute care setting.
For acute presentations requiring urgent medical assessment and care such as chest pain and shortness of breath, a site response strategy is required with immediate referral and pathways for seamless transfer to acute care services. Refer to Section 5: Health Wellbeing and Clinical Care for information on resident transfers to acute care services.
In quarantine, residents are restricted in the types of physical activity possible (relative to the facility characteristics) as part of disease transmission control, however physical activity should be made possible for residents and incorporated into service planning.
For quarantine services where residents have access to outdoor spaces, this may include walking around a mapped area with personal protective equipment (wearing masks).
There should also be the inclusion of insect repellent and sunscreen in residents’ rooms to ensure they can meet basic health safety needs whilst outdoors.
The attached physical activity resource for residents has been prepared by CNR physiotherapists to encourage physical activity within a quarantine facility noting restricted space, personal abilities and limited resources.
It is recommended this is provided for residents as part of their welcome pack.
Access the resource Section 4_Staying Active in Quarantine here.
People in quarantine and isolation are exposed to increased stress, anxiety and poor mental health, particularly at the beginning of disease outbreaks where there is often little known about disease transmission and characteristics.² Brief daily screening of residents’ health offers the opportunity for health staff to identify those who may be struggling with the quarantine setting and provide them with support and early intervention as required.
Quarantine Service mental health requirements:
- Understand that every person in quarantine is on their own journey and the reason they are in quarantine will likely affect their personal perspectives and ability to cope with isolation.
- Provide mental health services onsite (mental health nurse) with a referral pathway for teams working with residents.
- Establish pathways for acute services in case they are required, this includes access to a psychologist and identification of a close emergency department with mental health triage capabilities.
- Include observations of residents’ mental health and wellbeing as part of the daily resident health and wellness checking regime conducted by the Health Team.
- Ensure Telewellbeing services understand site mental health referral services and understand their responsibilities if they have a concerning conversation or communication with residents.
- Include mental health support contacts in resident information packs (e.g., Lifeline, Beyond Blue).
- Provide activities and recommendations to maintain mental health well-being in quarantine in resident information pack.
Access the resource Section 4_Keeping your mind and body healthy in quarantine.
Having access to information on quarantine requirements and the features of the quarantine service has been identified as a priority for residents along with information on travel restrictions, public health orders, disease monitoring and surveillance (for example viral screening processes such as swabbing).
Information needs to be written in clear English, interpreted where required (use an interpreter service), present core service contact points (reception, emergency, Telewellbeing Team), and be current.
A resident handbook, provided as both paper and online copies, is recommended along with a public-facing website that provides quarantine facility information and links to relevant government information sites.
A quarantine service social media site is advised, recognising people are generally comfortable navigating these and prefer the personal approach to information. Closed groups on sites such as Facebook are easy to establish but do require constant monitoring to respond to questions, resident feedback, and removal of any potentially offensive, false or misleading posts.
If in-house television is available in the quarantine facility, this presents another opportunity to provide site information and relevant public health and health promotion messaging.
Access the resource SECTION 4 Resident Quarantine Service Information
The quarantine environment needs to provide a safe space for residents where they are not at risk of disease transmission. Residents need access to equipment and information to ensure they are aware of their responsibilities to prevent infection. The site requires a strategy to support residents who become positive for a disease whilst in quarantine to ensure they are mentally and physically well and not a transmission risk to others. Refer to Section 2: Infection prevention and control – transporting infected residents for a guide on the management of the positive resident in quarantine.
Environmental approaches related to ventilation came to the forefront during the COVID-19 pandemic and highlighted measures to reduce the risk of disease transmission by utilising options such as: large open spaces with ventilation (open windows), MERV-13 air filters, portable air cleaners (with HEPA filters), and upper-room germicidal ultraviolet irradiation systems.³ High-risk activities with residents need to be planned to reduce disease transmission risk (such as conducting COVID-19 swabbing or during the resident arrival registration process).
Conducting these activities outdoors is ideal with the inclusion of appropriate personal protective equipment. Refer to Section 2: Infection prevention and control for further IPC guides.
Food becomes an area of focus for people in quarantine and often influences their overall quarantine experience.
There are three main considerations for residents in relation to their meals: quality, choices and distribution times.
Having the quarantine site provide all meals means residents lose autonomy related to their dietary intake and this can be balanced by organising click-and-collect (food delivery) services with local supermarkets.
Arrangements need to be in place to ensure items not permitted for residents onsite are not available for purchase and that food safety is maintained.
Quarantine provides an opportunity to offer healthy food options. A varied and healthy meal plan needs to accommodate standard, vegetarian, vegan, pescatarian, gluten free, lactose free diets as well as medical requirements such as diabetic meals, pregnancy safe or specific dietary requirements which allow for allergies and medical conditions. The menu should have age-dependent children’s meals that incorporate a smaller portion size and child-specific favourites.
Ideally, resident dietary requirements are collected prior to or on resident arrival and are best accommodated with onsite catering services.
Implementation of a welcome pack that provides a variety of snacks (not requiring refrigeration) and bottled water on arrival ensures immediate food needs are met.
Residents should be advised if they are able to drink tap water recognizing they may not be aware of this.
The quarantine staff are vital to the provision of resident care and the resident experience. Staff require education and training to enable them to provide support and care for residents, and be empathetic to residents’ circumstances.
Understanding residents will often be stressed and may experience anger at being quarantined requires additional staff preparation in resilience and navigating difficult situations.²
Staff should be informed on current infection prevention measures for disease control, government legislation, quarantine facility policies and strategies and most importantly be reactive to resident health priorities.
It is recommended that one team of staff work with a cohort of residents for the duration of their quarantine where possible, this provides continuity of care, facilitates awareness of individual resident characteristics and needs, and builds trust and rapport with residents.
Further information on quarantine staff can be found in Section 3: Health workforce.
A safe and healthy environment overlaps with every aspect presented in the resident-centred quarantine care model and includes privacy, personal safety, adequate room supplies, cleanliness and functionality of the quarantine environment.
Quarantine provides an opportunity for public health and health promotion actions and messaging. It can be viewed as a supportive environment, providing information and resources to inspire good health choices and improve health literacy, whilst protecting the greater community from disease transmission.
Most people in quarantine are not known to each other and unless people are traveling on international flights organised by the Department of Affairs, background police checks and criminal records are not accessed.
To facilitate a safe environment, the public health approach of organising residents into cohorts is recommended with three overarching actions:
- Keeping people traveling together cohorted together (for example everyone on one international flight would be considered a cohort) or by cohorting everyone arriving on the same date (used for domestic residents), this reduced the risk of exposure to other disease variants and infecting people who are at the end of their quarantine period.
- Separating groups within the cohort into families, couples and women traveling alone and men traveling alone.
- Placing families, couples and women traveling alone or any identified vulnerable residents closer to the security and staff entry point.
Rooms need to provide a private, comfortable, functional and safe environment. This means spaces such as family rooms consider aspects such as choking hazards, and rooms for people living with a disability are accessible with the required ramps, handrails and space to ensure comfort and functionality.
The core aspects for rooms are: private, clean, comfortable, accessible, furnished and accessorised, and ventilated to disease requirements.
To aid with keeping their room environment clean it is advised residents are provided with a basic cleaning pack which should include a bucket, dustpan and brush, cleaning/disinfectant wipes, cleaning clothes, and hand sanitiser.
Feeling culturally safe is a human right, and the quarantine facility needs to provide a service that acknowledges different cultural values. It is often beyond the scope of quarantine service provision to incorporate every individual cultural needs.
It is important that staff employed in the quarantine facility are culturally competent and capable to provide safe care to all the residents. This can be achieved by adopting cultural safety training for staff and promoting an inclusive service. The use of interpreters is critical and preparing materials in key languages of the cohorts in the quarantine facility where possible should be considered.
Consultation with Australia’s First Nations people is recommended to identify pathways for quarantine and isolation. In the establishment of a quarantine facility collaboration with local and national First Nations people will ensure a culturally appropriate environment is established within the quarantine facility.
Staff training in the journey of health and wellbeing recognising the unique challenges for Aboriginal and Torres Strait Islander peoples is recommended.
Communication with residents is central to residents feeling safe, informed and supported in their quarantine journey. Access to information before residents arrive to the quarantine facility alleviates the stress associated with entering an unknown environment.
Facilitating a communication cycle within the quarantine service empowers residents to have more control over their situation (even though they may be in mandated quarantine and isolation).
With the mass amount of information generated by social media in a pandemic, accessing and identifying relevant and true sources can be problematic for residents. Residents require access to current updates: local and national pandemic news, legislation and public health orders, transport arrangements, amount of time required for quarantine and exit dates. Two-way communication by means of phone, text messaging and face-to-face visits provides an opportunity for residents to be heard.
The health model of quarantine care includes a daily face-to-face health screen providing residents with an opportunity to communicate any concerns. In addition, telewellbeing calls or text messages are scheduled at least twice during the resident’s stay with the provision of a 24-hour contact phone number.
Ensuring residents have something to do in quarantine is important for mental health and wellbeing.
Access to entertainment in the form of television and reliable Wi-Fi systems featured heavily in CNR resident feedback accompanied by ideas on keeping children occupied, particularly when facing fourteen days of isolation.
Investing in children’s entertainment packs is recommended (containing age-appropriate games, books and a project such as lego or painting by numbers).
There are a number of activities that can be completed safely in quarantine and a list of these has been provided and should be included in the resident’s welcome pack.
Access the resource Section 4 Activities to keep you entertained in quarantine.
The resident journey
The journey through quarantine needs to be a coordinated and supportive process for residents. It can be divided into three separate areas of: resident arrival, management whilst in quarantine and resident departure. These areas have been briefly introduced below with a more comprehensive outline of processes and considerations presented in an attached document.
 There are three main teams of staff contributing to the resident journey:
There are three main teams of staff contributing to the resident journey:
- the health workforce
- Telewellbeing Teams (briefly outlined below)
- operations staff.
A full overview of their responsibilities in resident care can be found in Section 3: Health workforce.
The resident journey presented in this resource is modelled on the COVID-19 pandemic requiring a 14 day quarantine stay and incorporates viral screening identified as rapid antigen testing (RAT) and polymerase chain reaction (PCR).
The CNR utilised a telewellbeing service to provide an additional layer of resident support.
The Telewellbeing service was established offsite in the Department of Health. Telewellbeing teams included non-health professionals led by a health professional/clinical team leader (such as a registered nurse) and were provided with training to navigate difficult conversations, a script for resident wellbeing checks and referral pathways, and to understand the legalities and responsibilities of resident privacy and confidentiality.
The telewellbeing team form a crucial part of the resident journey often connecting with residents prior to their arrival in pre-arranged flights (such as repatriation flights). They continue to support residents throughout their stay with non-health matters, often flagging any residents with mental or physical health concerns to be followed up by the relevant onsite health professionals.
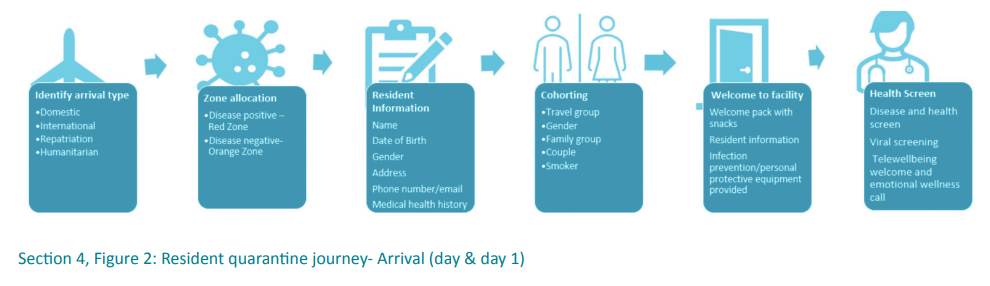
During the COVID-19 pandemic, residents arrived in quarantine both arranged as with repatriation flights or unexpectedly with flights quarantined mid-air due to changes in public health orders and government legislation or presenting a positive COVID-19 result with no suitable place to safely isolate.
The quarantine service is often presented with groups of residents to accommodate at short notice and requires a coherent approach to ensure rooms are available to facilitate cohorting, staff numbers are adequate to support residents, catering is aware and dietary requirements are accommodated. Resident welcome packs (with resident information and food) and IPC resources for residents need to be ready.
 On arrival to the service (or where possible prior to arrival), residents are cohorted and any dependents or vulnerable residents are identified.
On arrival to the service (or where possible prior to arrival), residents are cohorted and any dependents or vulnerable residents are identified.
Although luggage is not routinely searched a question to ensure no contraband enters the site is required. Experience from COVID-19 quarantine arrivals during the early stages of the pandemic found repatriation residents were not always open about their health issues due to fear of refusal of acceptance into quarantine.
Having a health team present for resident arrivals assists with screening residents’ health and identifying any who may require immediate or follow-up medical and/or mental health support.
Most importantly, online resident management information technology systems (RMITS) record every resident entering the facility with a required level of personal information adequate to keep them safe.
The RMITS needs to be a live, accessible and secure site where personal information can be safely stored. It is preferable that one RMITS serves across all site inclusive of: resident arrival type (domestic, repatriation, international, humanitarian, other), room allocation, room cleaning, catering (resident meal preferences), room allocation (and any room changes), resident information (personal information), quarantine requirements, and recording of resident interactions.
A separate site is recommended for resident health interactions to ensure resident confidentiality with personal health records.
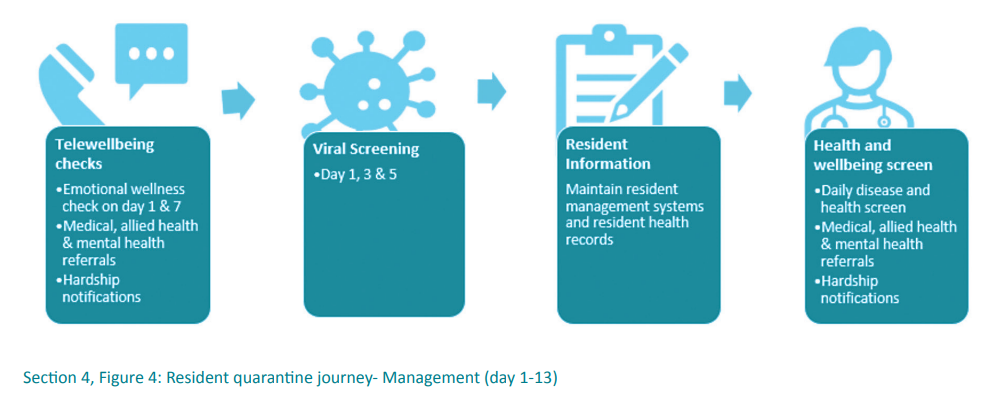
Once onsite residents are considered independent and self-caring, however they will require a number of interventions to ensure they are and remain healthy and safe. The health model approach of resident management incorporates a daily face-to-face visit from nurses to screen for disease signs and symptoms and check on general health and wellbeing (inclusive of mental health wellness).
Additional resident processes include viral screening in accordance with recommendations (this may involve screening on day one, three and five of quarantine), moving positive residents into a red zone (minimise risk to other residents), managing complaints, daily health checks and navigating requests for goods and services. Residents with special needs and hardship circumstances need to be identified and supported, which may include referral to other services such as social work or physiotherapy.
In exceptional circumstances day passes from quarantine may be issued for residents and these situations need to be navigated early to manage risk to the community.
Circumstances during COVID-19 in which these were granted were:
- Social emergencies- to attend a family funeral
- Medical emergencies- visit a terminally ill relative in the hospital
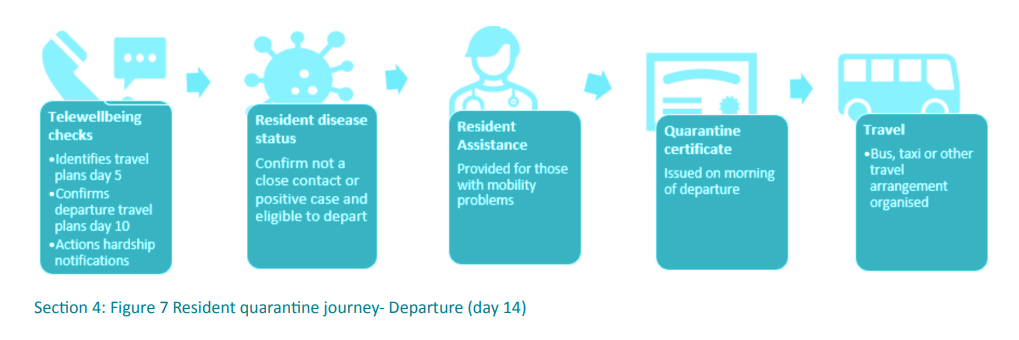
Clear communication with the residents about departure plans should commence early to identify residents with mobility requirements (wheelchair-bound or unable to climb bus steps) and other unique needs such as residents with hardship. Residents need to be aware of their departure date, the time they will be leaving and transport arrangements. It is recommended that this is officially commenced by day five and confirmed by day 10 for a 14 day quarantine.
The quarantine facility needs to provide certification of completed quarantine, particularly for international/repatriated residents and for those travelling on to other states and territories. The certificate is a doctor-signed statement of medical clearance from the facility and should be issued on the morning of a departure.
Evaluating the quarantine service provision from the resident perspective is important to understand if the resident centred model of care is effective. Surveys can be implemented during or at the completion of the residents stay and questions focussed on specific areas of the resident experience with the opportunity to provide written feedback. Areas a survey may focus on are: meals, sleep, physical activity options, medical care (if relevant), interactions with health teams, entertainment and the click and collect service. Additional areas can address personal safety (how safe residents feel in the facility) and how concerned they are with contracting the disease in the facility.
Surveys can also be used to determine the effectiveness of communication for residents and, gauge how the public health orders are being interpreted. All surveys should be anonymous and voluntary to complete.
Resident surveys can be distributed at anytime during their stay to determine how residents are settling into quarantine and highlight where the facility service and care provision needs to be reviewed. These can be provided as paper/hard copies to residents to complete and distributed/collected by the Health Team (noting paper cannot leave a red or orange zone and therefore photos of completed surveys are taken with the paper copy discarded at the doffing station). Alternatively, electronic versions can be emailed to residents by the Tele Wellbeing Team. It is noted that surveys are anonymous and voluntary for residents to complete.
Surveys can be used as a tool to assess how residents are adapting to border closures. For example, it was observed with border closures to states with large COVID-19 outbreaks residents were travelling between states by completing a period of quarantine in the Northern Territory enabling them to then enter a state (the state allowing NT entries). Adding a question to determine the reason residents were entering quarantine provides evidence of this behaviour which can then be used to inform strategies to reduce this burden on the quarantine service.
Question examples with a ranked response
- How satisfied are you with your sleep?
- How satisfied are you with your meals?
- How satisfied are you with the physical activity options?
- How satisfied are you with the entertainment options?
- How satisfied are you with the Welfare Outreach support provided to you?
- How satisfied are you with the click and collect process available to you?
- How happy are you with the medical care you are receiving?
- How concerned are you with contracting COVID19 virus?
- How satisfied are you that you are being protected from COVID19?
- Is the information provided to you daily appropriate to keep you informed?
Question examples with an open response
- Is there anything else we can consider providing you to support you during your stay?
- Would you like to speak to one or our Health Clinicians?
References
- Barriguete, M. O. F., & Zarasvand, S. A. (2021). Quarantine and COVID-19. J. Heal. Med. Nurs, 85, 7374. DOI: 10.7176/JHMN/85-11
- Henssler.J., Stock.F., van Bohemen.J., Walter.H., Heinz.A., & Brandt.L. Mental health effects of infection containment strategies: quarantine and isolation—a systematic review and meta-analysis. European Archives of Psychiatry and Clinical Neuroscience 271, no. 2 (2021): 223-234.
- Guo, M., Xu, P., Xiao, T., He, R., Dai, M., & Miller, S. L. (2021). Review and comparison of HVAC operation guidelines in different countries during the COVID-19 pandemic. Building and Environment, 187, 107368. https://doi.org/10.1016/j.buildenv.2020.107368
Content Acknowledgement
Content in this resource has been created and, in some cases, directly copied with permission from documents and resources owned and prepared by the Northern Territory Government, Department of Health, Centre for National Resilience, Howard Springs Quarantine Facility and the National Critical Care and Trauma Response Centre.
Reference this webpage (APA style guide)
To reference the webpage:
Charles Darwin University. (2023). Pandemic Quarantine Facility Guide. Top End Academic Health Partners. https://quarantine-guide.cdu.edu.au/
To reference a webpage document:
Charles Darwin University. (2023). Section 4 Resident care: The resident management process. Top End Academic Health Partners. https://quarantine-guide.cdu.edu.au/wp-content/uploads/2023/04/Section-4_Resident-management-process.pdf
Pandemic quarantine facility guide abbreviations and full reference list.