Infection prevention and control
A quarantine service functions with an assumption that all residents on entry could carry a disease of concern (such as COVID-19). There is a requirement to enforce staff and resident self-responsibility with safe infection prevention and control (IPC) behaviours.
An evidence-based set of IPC guidelines and equipment is required and this should be prepared and supported by dedicated and experienced IPC health professionals, with regular education and training. An IPC Committee is recommended to ensure the site is kept up to date with IPC advancements in response to evolving knowledge of disease aetiology and characteristics. These are additionally supported by disease surveillance, testing and contact management strategies and the Chief Health Officer’s Directions (considered law) and legislation so they can be enforced with the aim of public safety.
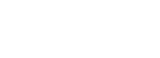
IPC strategies are recommended to incorporate the quarantine facility chain of infection to demonstrate the risk of transmission from the facility to the local community.
Quarantine facility chain of infection
In Australia during the COVID-19 pandemic quarantine and isolation was guided by the evidence-based guide provided by the Communicable Diseases Network Australia Series of National Guidelines (CDNA SoNG).1 This document is freely available online and has been updated regularly in accordance with advancements in disease understanding.

As the model of quarantine presented in this resource is based on a foundation of primary health care, the National Safety and Quality Health Service (NSQHS) Standards is another resource that presents the guidelines for the development of a high level of care and service provision within health services.2
This section of the quarantine and isolation toolbox presents core IPC recommendations including public health considerations, epidemiological directions, disease characteristics and transmission.
A complex overview of personal protective equipment (PPE), zones, viral screening and cleaning have been provided for adaption to different quarantine and isolation services.
Access the resource for the full Quarantine Pandemic Facility Guide Section 2.
Individual sections for Section 2: Infection prevention and control are presented with the information below.
Infection prevention and control toolbox
- hand hygiene
- physical distancing
- staying at home if unwell and seeking advice on viral screening.
- Covering the mouth and nose with a tissue when coughing or sneezing and turn your head away from others.
- Immediately disposing of the tissue.
- Performing hand hygiene with soap and water or use alcohol-based hand sanitiser (ABHS).
Understanding how a disease is affecting a population informs IPC practices and ensures the correct education and training can occur to arm quarantine staff with the knowledge required to protect themselves and the resident from disease.
This includes understanding the disease aetiology, transmission, and implementation of disease specific IPC processes.
The other important aspect of epidemiological studies is to identify the most vulnerable groups for whom disease transmission can potentially have dire consequences and implement measures to protect them.
This section of the resource presents those aspects of disease characteristics which need to be considered when preparing an IPC response to reduce risk of disease transmission.
The areas covered include:
- disease aetiology and transmission
- incubation periods
- disease signs and symptoms
- case definitions and contact definitions, all based on COVID-19.
Access the resource for Section 2_Disease aetiology and transmission.
Effective IPC in quarantine and isolation requires the support and participation of facility health staff.
The IPC committee consists of people who work together to promote a shared culture of safety and high-quality care across the site. The committee should have representatives from both the medical and non-medical staff and be prepared to coordinate the site’s IPC actions.
The key purpose of the committee is described as aiming to:
- Support all areas to fulfil their IPC responsibilities for ensuring the provision of high quality and safe resident care by oversight and responsibility of key objectives relating to the Australian Commission on Safety and Quality in Healthcare as they pertain to the quarantine facility, the Centre Disease Network Australian National Guidelines for Public Health Units and COVID-19 specific directions and guidelines.1,2
- To be responsible for oversight of educational strategies to actively promote principles of infection prevention and control and to ensure that effective work practices are maintained to prevent the spread of infectious diseases.
The following resource provides information about the committee roles and examples of agenda items.
There are designated zones within quarantine facilities and these require clear signage and mapped perimeters to ensure overall site safety. Zones are universally recognised to identity contaminated, potentially contaminated and uncontaminated areas and are designated ‘green’, ‘orange’ or ‘red’ based on communicable disease risk.
- Red zones are designated a contaminated area used for isolation, and the management of disease-positive cases (such as COVID-19 positive residents).
- Orange zones are designated as a potentially contaminated/infected areas used for routine quarantine, management of close contacts of disease-positive people and repatriation residents (noting these residents are considered international travellers and therefore pose a higher risk to the local community).
- Green zones are considered contamination free and this is the zone in which staff and offices are situated.
A complex overview of zones implemented in quarantine and isolation settings have been provided in the following attachment. This includes a more detailed definition of zones and the staff/resident management occurring in the orange and red zones inclusive of moving residents between zones.
The quarantine and isolation facility has the responsibility to provide appropriate and quality personal protective equipment (PPE) to its staff. During the COVID-19 pandemic there were many issues with lack of access to appropriate PPE with many clinical areas unable to sustain the level of PPE required during the COVID-19 pandemic.
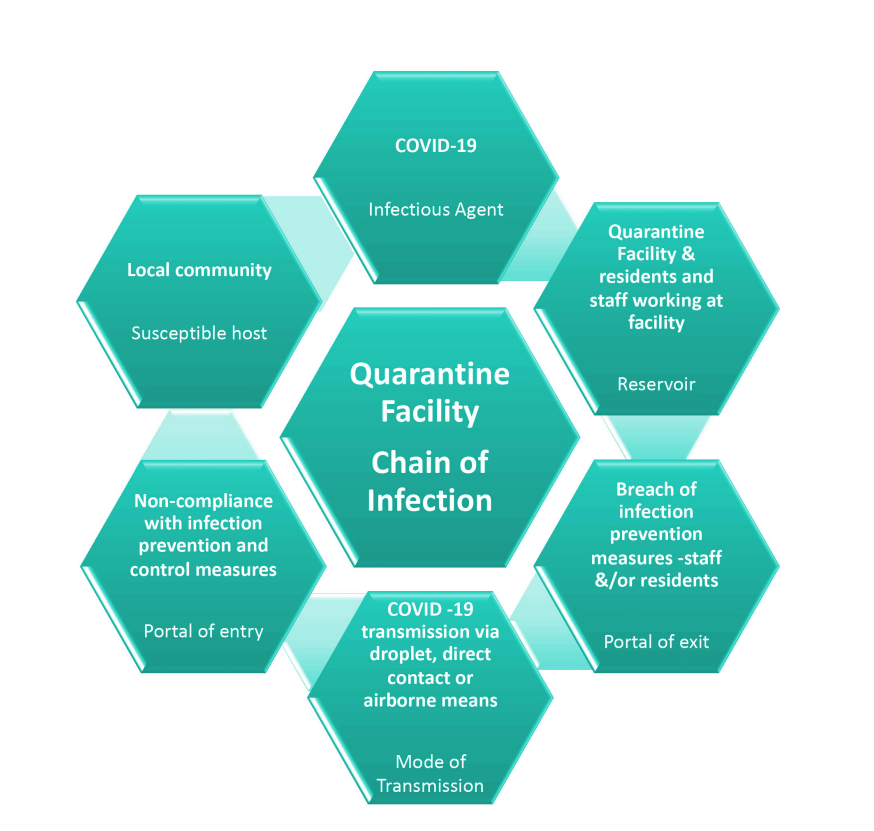
It is necessary to adapt levels of PPE to the epidemiology in the community and the facility. For example, PPE at quarantine facilities with outdoor resident management (such as that at CNR) are required to include consideration for weather elements.
Factors such as working in hot conditions in PPE present a risk for heat stress, and therefore time restrictions are required when wearing PPE. Other specific equipment such as N95 masks need to pass staff fit-testing whilst also being comfortable to wear.
Section 2: Figure 2: Centre for National Resilience, challenging environmental elements identified by staff when wearing personal protective equipment.
A full overview of PPE in quarantine and isolation which covers types of PPE, mask fit testing, guides for the different levels of PPE required (contact and non-contact roles), donning and doffing, PPE breaches management and PPE auditing has been provided.
Access the posters for donning and doffing PPE.
The potential risks associated with quarantine workers and residents contracting disease in the quarantine facility and subsequent spread to community settings are mitigated by a multifaceted prevention and management approaches.
Prevention is supported by a hierarchy of controls approach to mitigating the risk of transmission. The controls include mandatory site induction processes, personal protective equipment (PPE) training and refresher training and infection prevention controls, auditing across all work groups and locations on the site and enforcing of directions to residents in quarantine. During a pandemic with a communicable disease, viral screening of staff and residents becomes part of the routine risk management strategy.
The following guides present the delivery of high-quality, safe and appropriate screening and surveillance processes based on COVID-19 management in a quarantine facility. The aim is to prevent transmission and further spread through the early identification of disease-positive individuals. Viral screening is presented for both staff and residents.
Viral screening using approved tests is a tool to support the pandemic response but does not replace public health and hygiene measures that include site induction, PPE training for staff, standard precautions, hand hygiene and distancing requirements or vaccination and ongoing education of all staff and residents. This includes not coming to work if unwell and isolating if required to do so.
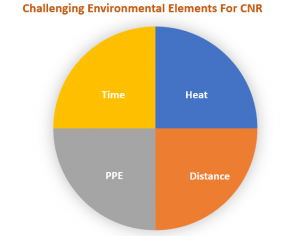
Disease transmission by direct contact with contaminated surfaces is preventable with good cleaning and disinfectant practices.
The role of cleaning is to reduce the number of infectious particles that may be present on a surface and therefore reduce the risk of transmission. Cleaning and disinfecting are not the same things.
- Cleaning involves physically removing dirt and organic matter from surfaces.
- Disinfecting involves the use of chemicals to eliminate germs on surfaces.
- It’s important to clean before disinfecting because organic matter and dirt can reduce the ability of disinfectants to eliminate germs.
Frequently touched surfaces such as bench tops, shared computers, door handles, light switches, toilets and taps need to be cleaned more regularly and then disinfected.
Recommendations during COVID-19 were that surfaces contaminated with respiratory droplets as a result of someone coughing should be immediately disinfected with the use of: disinfectants containing 70% + alcohol, hydrogen peroxide (oxygen bleach) or sodium hypochlorite (chlorine bleach) for hard surfaces. Disinfectants also must remain on a surface for enough time to eradicate the virus particles and this can be found in various product recommendations.4
A full resource presenting considerations and methods to clean across the quarantine site (including resident zones) has been presented here. It is recommended that for the purpose of environmental cleaning, the resource prepared by the Australian Commission on Safety and Quality in Health Care Principles of environmental cleaning: product selection is also consulted.5
Fact sheet- Principles of environmental cleaning: product selection|Australian Commission on Safety and Quality in Health Care.
The process for managing the removal of waste is covered in the Section 1: Processes, infrastructure and communication.
From the IPC perspective, the following core points need to be followed:
- Biohazard waste goes into yellow biohazard bags and is managed in accordance with approved processes and procedures. PPE waste at doffing stations is collected as clinical waste.
- All other waste is treated as general waste and managed by the facilities manager.
- Residents are responsible to remove their waste from their rooms, including disposing off the waste generated by the food supply. Waste bins are provided in each resident area.
- Waste bins are collected from the resident zones by a contractor, with staff wearing appropriate PPE.
- Waste collected during the process of swabbing is collected in clinical waste bags and later treated as general waste as per guidelines.
All waste management approaches need to consider the environmental impact (sustainable practice), and costs, and aim to improve health and safety (reduces the risk of spreading infection).
Auditing forms a core part of site quality assurance practices and ensures processes are working as planned.
For IPC purposes auditing is focused on:
- IPC and PPE training and education
- hand hygiene
- PPE: equipment procurement, quality and purpose, donning and doffing, fit testing.
- staff vaccination: number of vaccinations acquired and number administered (noting any wastage), staff vaccination compliance, staff who are able to administer vaccinations, AIR, AIEFs.
- cleaning: techniques/processes and their outcomes, equipment, staff and resident areas.
- Viral screening/ Swabbing: residents and staff swabbing compliance, techniques/processes, and equipment. Positive results and outcomes.
It is recommended that all quarantine staff have an electronic ID card. This ID card is used for IPC monitoring (entry to site, staff viral screening and meal areas). This provides an audit trail of arrival, departure, testing and measures congregation on site and being tested that is monitored by the audit team and can be matched against gate entry and exits. This also provided important information if onsite contact tracing is required.
Each agency and contractor is responsible to ensure their staff, subcontractor’s staff and/or approved visitors are added to the CNR swab list and undertake swabbing when on site. Visitors are registered under the agency or contractor providing for their supervision on site.
Spot checks and auditing occurs across the site, including the Green Zone to promote the hierarchy of controls for reducing disease transmission. The focus remains on ongoing education and support with escalation to the agency or contractor lead of issues or concerns regarding their staffing cohort for resolution.
References
- Australian Government, Department of Health and Aged Care. CDNA Series of National Guidelines. Communicable Diseases Network Australia Series of National Guidelines (CDNA SoNG).
- Australian Commission on Safety and Quality in Health Care. National Safety and Quality Health Service (NSQHS) Standards.
- World Health Organisation (2009). WHO guidelines on hand hygiene in health care.
- Government of South Australia (2021) Cleaning Standard for South Australian Healthcare Facilities.
- Australian Commission on Safety and Quality in Health Care. (2022). Fact sheet- Principles of environmental cleaning: product selection.
Content acknowledgement
Content in this resource has been created and, in some cases, directly copied with permission from documents and resources owned and prepared by the Northern Territory Government, Department of Health, Centre for National Resilience, Howard Springs Quarantine Facility and the National Critical Care and Trauma Response Centre.
Reference this webpage (APA style guide)
To reference the webpage:
Charles Darwin University. (2023). Pandemic Quarantine Facility Guide. Top End Academic Health Partners. https://quarantine-guide.cdu.edu.au/
To reference a webpage document:
Charles Darwin University. (2023). Section 2 Infection prevention and control: Viral screening. Top End Academic Health Partners. https://quarantine-guide.cdu.edu.au/wp-content/uploads/2023/04/Section-2_Viral-Screening.pdf
Pandemic quarantine facility guide abbreviations and full reference list.